SLU Researcher Reports Improvements in Survival Rates in Patients with Metastatic Prostate Cancer
ST. LOUIS — Research from Saint Louis University School of Medicine finds improvements in survival in both veterans and men across the country over the last 20 years in metastatic prostate cancer, which correlates with new hormonal treatments.
Martin Schoen, M.D., assistant professor of medicine and a member of the Saint Louis University AHEAD Institute, quantified trends in overall survival among men newly diagnosed with metastatic prostate cancer and has revealed his findings in a recent research letter in JAMA Network Open.
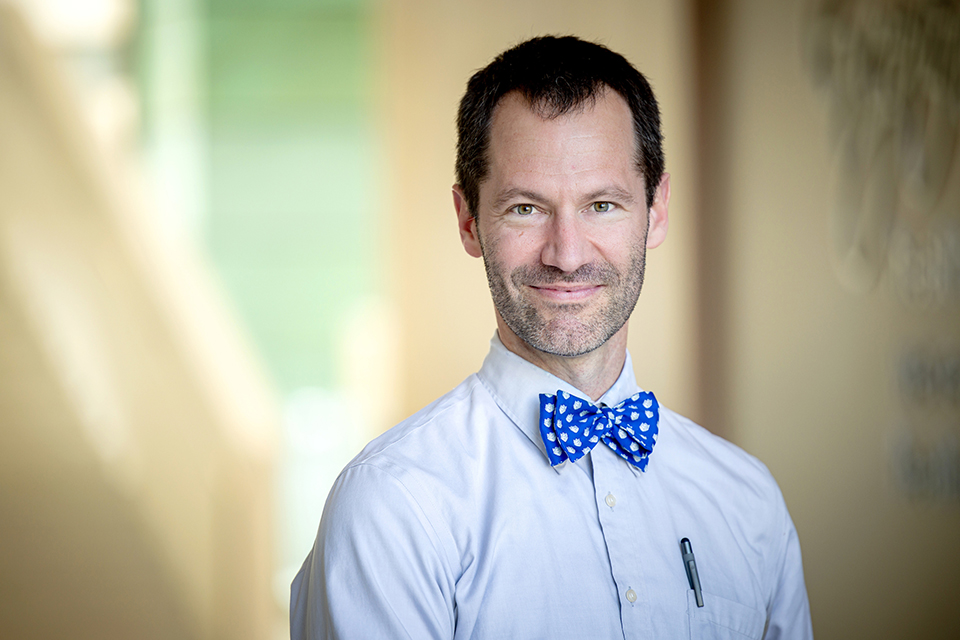
Martin Schoen, M.D., assistant professor of medicine and a member of the Saint Louis University AHEAD Institute. Photo by Sarah Conroy.
Metastatic prostate cancer accounts for 5–10% of all prostate cancer diagnoses, but it is responsible for nearly 50% of prostate cancer-related deaths. Since 2015, the prognosis of metastatic prostate cancer has improved with the introduction of new hormonal treatment and chemotherapy combined with androgen deprivation therapy in the first-line setting.
“In the last 10 years, several new therapies have been created that have made a dramatic impact in clinical trials,” said Schoen, lead author of the study. “We wanted to study this in the general population to assess whether these breakthroughs were making its way to them.”
The study reviewed two national datasets to identify the health outcomes of men with prostate cancer, one of the most common cancers in veterans. The cross-sectional retrospective study included male patients first diagnosed with prostate cancer between the years 2000-2019. Schoen and his team analyzed datasets of 58,859 men from SEER (Surveillance, Epidemiology, and End Results) and 14,904 men from the Veterans Affairs Central Cancer Registry (VACCR).
The SEER Program of the National Cancer Institute (NCI) collects and publishes cancer incidence and survival data from population-based cancer registries covering about 48% of the U.S. population. The VACCR collects cancer diagnosis and treatment information from the 132 VA Medical Centers that treat veterans with cancer.
The study focused on the survival of men in different age groups. Schoen and the research team found that the median overall survival in patients younger than 70 significantly improved in the U.S. population from 2000 to 2019. Still, there was little change in men over 70 during the same period.
The study also found that overall survival rates were similar in SEER and VHA. Schoen, a Navy veteran who works as a hematologist/oncologist at St. Louis Veterans Affairs Medical Center, said he was pleased the data showed that in prostate cancer care, veteran care is as good or better than the treatment men receive in the general community.
The study notes that while new treatments are available and increased overall survival has been observed in clinical trials, researchers cannot assume these developments improve disease management in clinical practice. The overall survival of men with metastatic prostate cancer is lower in clinical practice than in clinical trials, as patients are typically older with more health conditions.
Researchers say further study is needed as the study is limited by lack of data on men with other medical problems, such as heart disease or diabetes.
This study was supported by the Prostate Cancer Foundation Igor Tulchinsky, Robert Taubman Sandler – PCF Valor Young Investigator Award, and Department of Defense grant No. W81XWH-22-1-0602.
Additional authors include Bruce Montgomery, M.D., VA Puget Sound Healthcare System, Fred Hutchinson Cancer Center and University of Washington School of Medicine; Lukas Owens, VA Puget Sound Healthcare System and Fred Hutchinson Cancer Center; Saira Khan, Ph.D., Washington University in St. Louis School of Medicine; Kristen Sanfilippo, M.D., Washington University in St. Louis School of Medicine; and Ruth B. Etzioni, Ph.D., Fred Hutchinson Cancer Center and University of Washington School of Medicine.
Latest Newslink
- A Camp Friendship that Stirred Up Lifelong BondsIn the summer of 2005, Mary Kate Keenoy (Chaifetz Grad '22) and Genevieve Willman met at SLU's Gardens to Tables culinary camp. What started as a shared interest in cooking grew into a lasting friendship that has endured for two decades.
- Bruce Bacon, M.D.: 1949-2025Bruce Bacon, M.D., professor emeritus of internal medicine, died Sunday, July 6, 2025. He was 75. Bacon was known globally for his expertise in all aspects of clinical hepatology, specifically hemochromatosis, viral hepatitis, chronic liver disease / general hepatology, and liver transplant. Bacon was also a member of the research team that discovered the gene for hemochromatosis, HFE, in 1996.
- SLU Launches William L. Clay, Sr. Institute of Civic Engagement and Economic JusticeThe Clay Institute will provide immersive learning experiences and hands-on training that address the social and economic challenges facing the St. Louis region and the nation. Institute programming will be available to all students with an interest in civic engagement and democratic participation.
- SLU Research Explores Depression's Ripple Effect on DiabetesA study conducted by researchers at Saint Louis University found that patients with depression were more likely to have uncontrolled diabetes over time and that depression contributes to a heightened economic burden to diabetes management.
- SLU/YouGov Poll: Statewide Cell Phone Ban for Missouri Schools Popular with VotersGovernor Mike Kehoe has signed Senate Bill 68 into law, enacting a statewide ban on the use of personal electronic devices, including cell phones, tablets, and smartwatches, throughout the school day in Missouri public and public charter schools.
- SLU Vaccine Center Will Enroll Healthy Volunteers in Yellow Fever Vaccine Clinical TrialSaint Louis University's Center for Vaccine Development will enroll up to 70 adult volunteers in a clinical trial to study the safety elicited by a new investigational vaccine for yellow fever, a potentially deadly disease that is spread by mosquitoes. The research is funded by Sanofi Pasteur.